
The treatment of patients with bradycardia and hypotension begins with fluids and atropine, but patients who are more than mildly poisoned typically do not have an adequate response to these therapies. Even at therapeutic doses, the ingestion of more CCB or β-blocker medication than is prescribed can be life-threatening in a patient with a tenuous cardiac history.īecause of the pathophysiologic similarities of CCB toxicity and β-blocker toxicity, their management is similar.
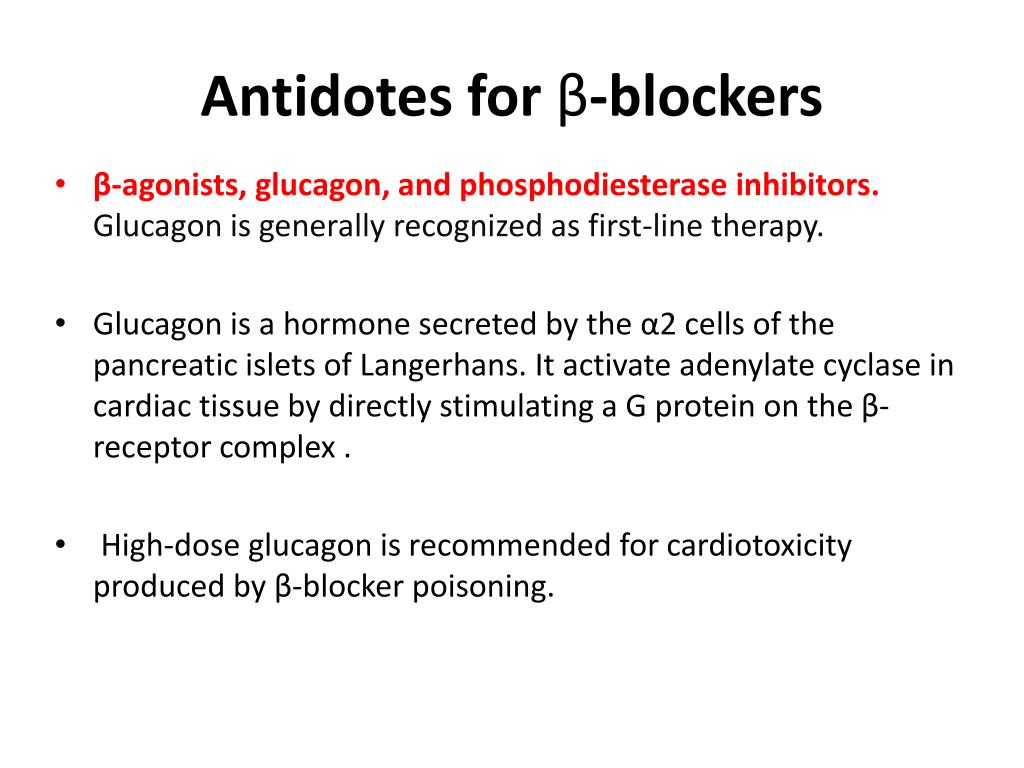

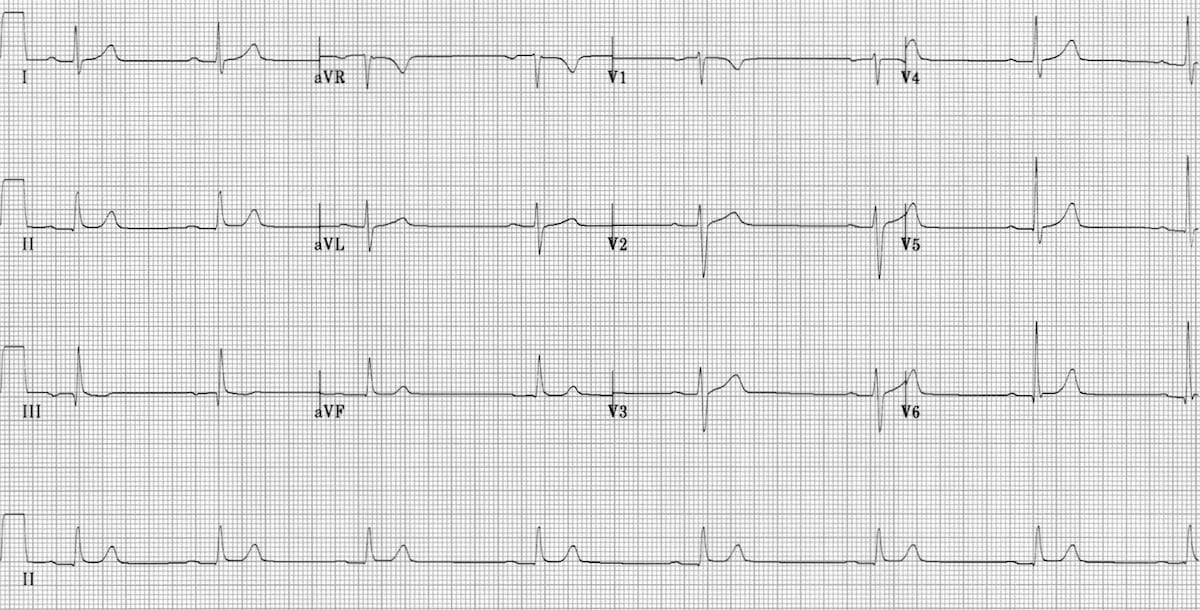
Toxicity resulting from the ingestion of the combination of a β-blocker and a CCB can be particularly serious and life-threatening. Propranolol, a β-blocker with high lipophilicity and sodium-channel-blocking effects, is more likely than other β-blockers to cause patients to have a seizure and to exhibit a widened QRS complex on electrocardiography. Dihydropyridine CCBs such as nifedipine are more potent peripheral vasodilators than nondihydropyridine CCBs they have limited effects on cardiac rhythm and are more likely to cause hypotension with reflex tachycardia. Children experiencing a β-blocker overdose may develop hypoglycemia, an uncommon symptom in adults. The more severe the CCB overdose, the more likely the patient is to exhibit hyperglycemia, because CCBs also inhibit the release of insulin from pancreatic β-cells via a calcium-dependent pathway. Patients experiencing a CCB overdose tend to remain awake and alert, even in the event of profound hypotension and bradycardia, while patients with β-blocker poisoning are more likely to have an altered mental status and respiratory depression. Subtleties in presenting symptoms can help differentiate CCB and β-blocker poisoning.


 0 kommentar(er)
0 kommentar(er)
